Abstract
Background Heparin-induced thrombocytopenia (HIT) is a complication of heparin exposure with potential for significant morbidity and mortality. The serotonin release assay (SRA) has been considered the gold standard for HIT diagnosis. However, the SRA is technically challenging and results can be influenced by specimen handling and preparation. Therefore, the performance of the real-world assays may differ from published standards but reports of real-world performance are not widely available. A new assay, the PF4-dependent P-selectin expression assay (PEA), has demonstrated comparable accuracy in HIT diagnosis employing a simpler laboratory technique. Herein, we report the real-world performance of a reference laboratory SRA and PEA and describe how incorporation of the PEA into the testing algorithm positively influenced the HIT diagnostic process at a large academic medical center.
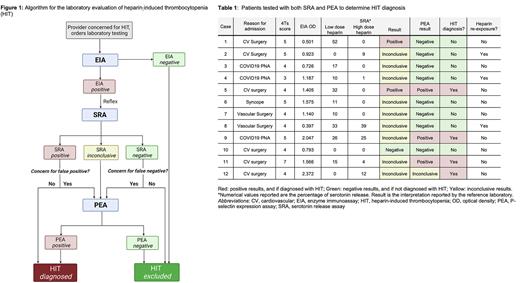
Methods At the University of Alabama at Birmingham, we incorporated the PEA into HIT testing at provider discretion in patients with inconclusive SRA results starting January 1, 2020. Since July 15, 2020, we solidified the use of PEA in our algorithm (Figure 1) in which all patients with an inconclusive SRA had a PEA on the same specimen. A PEA could also be ordered ad hoc if the SRA result did not correlate with clinical suspicion for HIT.
We retrospectively compared patients tested for HIT for 2 years before PEA use (January 1, 2018 to December 31, 2019; pre-PEA period) to the >2 years since using the PEA (January 1, 2020 to March 1, 2022; PEA period). All patients tested with PEA at our institution are included in Table 1.
Laboratory testing: Enzyme immunoassay (EIA) was performed at our institution using Asserachrom® HPIA, Diagnostica Stago (France). The SRA and PEA assays were performed at Versiti (Milwaukee, WI). SRA was positive if there was >20% release of serotonin with low dose heparin (0.1 U/mL) and <20% release in with high dose heparin (100 U/mL). An inconclusive result was defined as a percentage of serotonin release not meeting criteria for a positive result (e.g., >20% release of serotonin with both low and high dose heparin, or some release but <20% with low dose along with inhibition with high dose).
Statistical analysis
Descriptive statistics were employed to examine the sample of patients with an inconclusive SRA result, comparing those with and without PEA testing. Bivariate analyses were conducted to compare testing patterns in the pre-PEA and PEA periods, and T-tests of significance were conducted to analyze assay results. All models were estimated using Stata 17 (StataCorp. 2019. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC).
ResultsSRA results: In the pre-PEA and PEA periods, there were 1,252 and 1,403 EIAs performed, respectively. The rate of EIA positivity was similar in both groups (14% vs 15%, p=0.813). A total of 379 SRAs were sent in both periods, with 24 inconclusive results (6%, 15 pre-PEA and 9 PEA).
PEA performance: In the 24 patients with inconclusive SRA results, HIT was diagnosed in 7 of 15 patients (47%) pre-PEA, compared to 3 of 9 patients (33%) in the PEA period. Table 1 presents the details of each case where PEA was used due to diagnostic uncertainty. Of the 9 patients with an inconclusive SRA result in the PEA period, PEA provided a definitive result in 8 cases (89%). In 2 cases, the PEA confirmed the SRA result, 1 positive and 1 negative. In 1 case with a positive SRA and low clinical suspicion, the PEA was negative.
Conclusion Evaluation of the real-world performance of the SRA reveals that although inconclusive results are rare (6%), they can present a significant diagnostic challenge in centers with high testing volume. The PEA demonstrated reliable performance in patients with an inconclusive SRA, producing a definitive result in 89% of cases. The percentage of patients diagnosed with HIT after an inconclusive SRA result decreased with incorporation of the PEA (47% to 33%), suggesting that PEA use helped refute a HIT diagnosis when there was clinical uncertainty. Further studies are needed to determine the optimal testing algorithm to produce rapid, reliable HIT diagnosis.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal